Merrillville, IN
Munster, IN

What Are Gout Tophi?

Gout is a type of arthritis caused by a buildup of uric acid in the bloodstream. This acid can crystallize and become lodged in the joints of the feet, particularly the big toe, leading to sudden and intense pain, swelling, and inflammation. Gout typically flares up and then goes away, only to flare up again. It can become a chronic condition if measures are not taken to prevent future flare-ups. Chronic gout can cause large, visible bumps, called tophi, to form in bones, joints, or cartilage. Tophi are made of urate crystals and are usually not painful unless they become infected or press on a nerve. But although they’re not painful in and of themselves, tophi are problematic because they can damage joints, destroy cartilage, and eventually lead to bone erosion, deformity, and disability. For more information about gout, it is suggested you consult with a podiatrist.
Gout is a painful condition that can be treated. If you are seeking treatment, contact Ahmad Elsamad, DPM from The Institute of Foot & Ankle Reconstructive Surgery . Our doctor will treat your foot and ankle needs.
What Is Gout?
Gout is a form of arthritis that is characterized by sudden, severe attacks of pain, redness, and tenderness in the joints. The condition usually affects the joint at the base of the big toe. A gout attack can occur at any random time, such as the middle of the night while you are asleep.
Symptoms
- Intense Joint Pain - Usually around the large joint of your big toe, and it most severe within the first four to twelve hours
- Lingering Discomfort - Joint discomfort may last from a few days to a few weeks
- Inflammation and Redness -Affected joints may become swollen, tender, warm and red
- Limited Range of Motion - May experience a decrease in joint mobility
Risk Factors
- Genetics - If family members have gout, you’re more likely to have it
- Medications - Diuretic medications can raise uric acid levels
- Gender/Age - Gout is more common in men until the age of 60. It is believed that estrogen protects women until that point
- Diet - Eating red meat and shellfish increases your risk
- Alcohol - Having more than two alcoholic drinks per day increases your risk
- Obesity - Obese people are at a higher risk for gout
Prior to visiting your podiatrist to receive treatment for gout, there are a few things you should do beforehand. If you have gout you should write down your symptoms--including when they started and how often you experience them, important medical information you may have, and any questions you may have. Writing down these three things will help your podiatrist in assessing your specific situation so that he or she may provide the best route of treatment for you.
If you have any questions, please feel free to contact our offices located in Merrillville, and Munster, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Gout
Gout is a form of arthritis that is caused by a buildup of uric acid crystals in the joints. This considered to be one of the most frequently recorded medical illnesses throughout history. Gout occurrences in the US have risen within the past twenty years and the condition now affects 8.3 million people which is 4% of all Americans. Researchers have found that gout affects men more than women and African-American men more than white men.
Symptoms of gout are warmth, swelling, discoloration, and tenderness in the affected joint area. The small joint on the big toe is the most common place for a gout attack to occur.
People who are obese, gain weight excessively, drink alcohol heavily, have high blood pressure, or have abnormal kidney function are more likely to develop gout. Furthermore, certain drugs and diseases are likely to increase levels of uric acid in the joints which eventually leads to gout. You are also more likely to develop gout if you eat a lot of meat and fish.
Many who experience gout attacks will experience repeated attacks over the years. Some people who have gout symptoms, may never have them again, but others may experience them several times a year. If you have gout symptoms throughout the year, you may have recurrent gout. Those who have gout should also be careful about their urate crystals collecting in their urinary tract, because this may lead to kidney stones.
Diagnosis for gout is done by checking the level of uric acid in the joints and blood. Your podiatrist may also prescribe medicine to reduce uric acid buildup in the blood, which will help prevent any gout attacks.
To treat gout, your podiatrist may also prescribe you Anti-inflammatory medication (NSAIDs) which will relieve the pain and swelling of a gout episode and it can also shorten a gout attack. Maintaining a healthy diet is also a proven method to prevent gout attacks.
Diabetic Foot
 Diabetic foot is a term used to describe complications that affect the feet of individuals with diabetes. These complications arise from poor blood circulation and nerve damage, or neuropathy, caused by high blood sugar levels. As a result, minor injuries or sores can go unnoticed and become infected, leading to severe issues, such as ulcers or even amputation, if left untreated. Individuals at risk for diabetic foot include those with poorly controlled diabetes, a history of foot ulcers, or existing peripheral neuropathy. People with diabetes who smoke, have high blood pressure, or high cholesterol are also at increased risk due to impaired blood flow to the extremities. Treatment involves a comprehensive approach, including regular foot inspections, proper wound care, blood sugar management, and wearing appropriate footwear to prevent injury. In severe cases, medical interventions like debridement, antibiotics, or surgery may be required. If you have diabetes, it is strongly suggested that you are under the care of a podiatrist who can counsel you on preventive care, provide routine check-ups, and treat any foot problems that may arise.
Diabetic foot is a term used to describe complications that affect the feet of individuals with diabetes. These complications arise from poor blood circulation and nerve damage, or neuropathy, caused by high blood sugar levels. As a result, minor injuries or sores can go unnoticed and become infected, leading to severe issues, such as ulcers or even amputation, if left untreated. Individuals at risk for diabetic foot include those with poorly controlled diabetes, a history of foot ulcers, or existing peripheral neuropathy. People with diabetes who smoke, have high blood pressure, or high cholesterol are also at increased risk due to impaired blood flow to the extremities. Treatment involves a comprehensive approach, including regular foot inspections, proper wound care, blood sugar management, and wearing appropriate footwear to prevent injury. In severe cases, medical interventions like debridement, antibiotics, or surgery may be required. If you have diabetes, it is strongly suggested that you are under the care of a podiatrist who can counsel you on preventive care, provide routine check-ups, and treat any foot problems that may arise.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Ahmad Elsamad, DPM from The Institute of Foot & Ankle Reconstructive Surgery . Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our offices located in Merrillville, and Munster, IN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
How to Care for Diabetic Foot
Millions of people are affected by diabetes each year. Diabetes damages blood vessels in all parts of the body, especially the feet. The legs and feet may develop slow blood flow, which causes neuropathy, or nerve damage. Once a diabetic patient develops neuropathy, it is important that the feet are well taken care of. Otherwise, the lower limbs may have to be amputated. This only happens in drastic cases, but it shows how seriously diabetic foot care should be taken.
It is very important to always wash and dry the feet thoroughly, especially in between the toes, if you’re a diabetic. Secondly, examining your feet and toes for redness or sores must be done, even if you do not feel pain. You may also want to examine your feet from the bottom. Try to avoid wearing colored socks to prevent infections that may occur from the dye. Well-fitting socks are also highly recommended.
A diabetic’s physician should always monitor their blood levels to test how well blood sugars are being maintained. In addition to giving advice about everyday eating habits and foot care, a physician may prescribe medicine to help with the diabetic patient’s neuropathy. It is also advised to see a podiatrist if experiencing any feet conditions. Toenails may also need to be taken care of by a podiatrist. This prevents patients from cutting too deeply around their cuticles, which can lead to infection.
A person can take care of their feet at home by following the instructions of their physician. Using creams on one’s feet is also an effective way to heal dryness. Proceed with caution when using tools to remove calluses, as severe diabetics may not be able to feel pain on their feet. If any complications arise do not hesitate to contact a podiatrist.
On a daily basis, diabetic feet must be checked. If you are ever concerned about something, contact your health care professional. You never want to wait until a wound becomes too severe to treat. If left untreated, gangrene may develop. Gangrene is a serious infection that can lead to sepsis or amputation. It is also important for diabetics to be on the lookout for ulcers. Ulcers are sores that develop from tissue loss on the skin. They can be quite painful and require intensive treatment. Early treatment and everyday inspection are imperative to staying healthy.
Treating Athlete’s Foot
 Athlete's foot, or tinea pedis, is a common fungal infection that affects the skin of the feet. It is caused by dermatophytes, fungi thriving in warm, moist environments like shoes, locker rooms, and swimming pools. Symptoms can include itching, stinging, and burning between the toes or on the soles, in addition to blisters, cracking, peeling, and dry skin. Risk factors include walking barefoot in communal areas, sharing footwear, having sweaty feet, and wearing tight-fitting shoes. People with weakened immune systems or diabetes are particularly susceptible. Treatment involves antifungal medications, available as creams, sprays, powders, or oral medications. Keeping feet clean and dry, changing socks regularly, and using antifungal powders can prevent recurrence. Complications can arise if left untreated, such as secondary bacterial infections, spreading to other body parts, and chronic infection. If you have a severe case of athlete’s foot, it is suggested that you visit a podiatrist for more aggressive treatment and medical supervision.
Athlete's foot, or tinea pedis, is a common fungal infection that affects the skin of the feet. It is caused by dermatophytes, fungi thriving in warm, moist environments like shoes, locker rooms, and swimming pools. Symptoms can include itching, stinging, and burning between the toes or on the soles, in addition to blisters, cracking, peeling, and dry skin. Risk factors include walking barefoot in communal areas, sharing footwear, having sweaty feet, and wearing tight-fitting shoes. People with weakened immune systems or diabetes are particularly susceptible. Treatment involves antifungal medications, available as creams, sprays, powders, or oral medications. Keeping feet clean and dry, changing socks regularly, and using antifungal powders can prevent recurrence. Complications can arise if left untreated, such as secondary bacterial infections, spreading to other body parts, and chronic infection. If you have a severe case of athlete’s foot, it is suggested that you visit a podiatrist for more aggressive treatment and medical supervision.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet and ankles, contact Ahmad Elsamad, DPM from The Institute of Foot & Ankle Reconstructive Surgery . Our doctor will treat your foot and ankle needs.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
- Hydrate your feet by using lotion
- Exfoliate
- Buff off nails
- Use of anti-fungal products
- Examine your feet and visit your doctor if any suspicious blisters or cuts develop
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact our offices located in Merrillville, and Munster, IN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Athlete’s Foot
Athlete’s foot, or tinea pedis, is a skin disease caused by a fungal infection. The infection typically occurs between the toes, and the feet are most subject to this disease because shoes best create the warm, dark, and moist environment in which fungus thrives. Other areas that create a similar environment, such as swimming pools, public showers, and locker rooms; can also promote fungi growth.
Symptoms of athlete’s foot include dry skin, itching, scaling, inflammation, and blistering. Sometimes, blisters can evolve into the cracks or breaks in the skin. The exposed tissue can then create pain, swelling, and discharge. The spread of infection can cause itching and burning as well.
While athlete’s foot commonly occurs between the toes, it may also spread to the toenails or soles of the feet. Other parts of the body, such as the groin or underarms, can also become infected if they are touched after the original area of infection is scratched. Aside from physical contact, athlete’s foot can also spread through the contamination of footwear, clothing or bedsheets.
Proper foot hygiene is essential in preventing athlete’s foot. You can prevent the fungus from spreading by frequently washing your feet using soap and water, thoroughly drying the feet between the toes, changing shoes and socks every day to reduce moisture, and ensuring that bathroom and shower floors are disinfected. Other tips include using shower shoes, avoiding walking barefoot in public environments, wearing light and airy shoes, and wearing socks that keep the feet dry.
While treatment for athlete’s foot can involve topical or oral antifungal drugs, mild cases of the infection can be treated by dusting foot powder in shoes and socks. Any treatment used can be supplemented by frequently bathing the feet and drying the toes. If proper foot hygiene and self-care do not ease your case of athlete’s foot, contact your podiatrist. He will determine if the underlying cause of your condition is truly a fungus. If that is the case, a comprehensive treatment plan may be suggested with the inclusion of prescription antifungal medications.
Are You Suffering From Ingrown Toenails?
Exercises That Can Help Seniors to Prevent Falling

Falls are a significant concern for seniors, with someone aged 65 or older experiencing a fall every second. Falls are the leading cause of injury-related death in this age group. To help prevent falls, focusing on exercises that strengthen the feet and improve balance is essential. Strengthening the muscles in your feet can enhance stability and support. Simple exercises like toe curls, where you pick up small objects with your toes, can significantly improve foot strength. Another effective exercise is heel-to-toe walking, which enhances balance by promoting coordination and proprioception. Practicing ankle circles and calf raises can also improve flexibility and strength in the lower legs and feet. Incorporating balance exercises, such as standing on one leg or using a balance board, can further reduce the risk of falls by training your body to maintain stability. It is important to check with a podiatrist before undertaking a course of exercises related to falling. For guidance on methods to prevent falling, it is suggested that you schedule an appointment with a podiatrist for an exam, diagnosis, and treatment options.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with Ahmad Elsamad, DPM from The Institute of Foot & Ankle Reconstructive Surgery . Our doctor will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our offices located in Merrillville, and Munster, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Falls Prevention
Elderly Americans are very susceptible to falls as they get older. Everyone experiences decreases in flexibility, balance, strength, and the senses as they age. This correlates to some eye-opening statistics. 1 in 4 Americans aged 65 and older fall each year. An elderly American is being treated for a fall in an emergency room every 11 seconds. In light of these striking statistics, one can see the importance of taking steps to prevent falls.
Finding an exercise program for the elderly is an excellent way to reduce the likelihood of falls. Look for an exercise program that improves strength and balance. Elderly people who live a more sedentary lifestyle, with little physical activity, are at an increased risk of falling. Wearing well-fitted footwear that provides good foot support and cushion will help prevent falls from poorly fitted shoes. Talking to a podiatrist about your susceptibility to falls and about inspecting your prescriptions will help to avoid any medication that could make falls more likely. Due to a decline in the senses among the elderly, having your eyes and hearing checked is recommended.
Around half of all falls occur in the household. Removing tripping hazards in the home and making it more accommodating to older persons can significantly reduce falls. Some notable household changes include increasing lighting around the house, installing grab bars in the shower and bathroom, and making sure the floor is clear of clutter. Other smart options include installing a shower chair, using rubber-bottomed rugs, and placing railings on both sides of stairwells.
Finally, discuss with a doctor and your family about your fear of falling. This will help to increase awareness among the population on the need for fall prevention. A lack of awareness on the matter, and a downplaying of importance are what increase the risks of falling. Following these tips can help to reduce the risk for yourself and your loved ones.
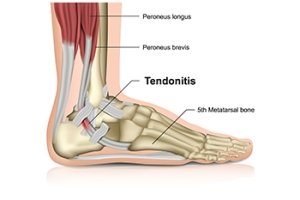
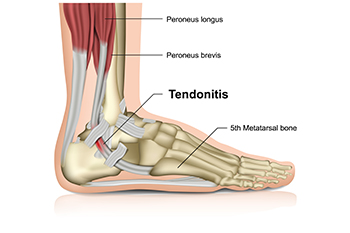
Causes and Relief Options for Achilles Tendonitis
Achilles tendonitis is an inflammation of the Achilles tendon, the band connecting the calf muscles to the heel bone. This condition often arises from overuse, such as repetitive stress from activities like running or jumping. It can also result from a sudden increase in exercise intensity, wearing poor footwear, or tight calf muscles. Symptoms can include pain and stiffness along the tendon, especially in the morning or after physical activity. Relief options focus on reducing inflammation and promoting healing. Resting the affected foot can alleviate pain and swelling. Taking anti-inflammatory medications can also help to provide additional relief. Gentle stretching and strengthening exercises may restore flexibility and prevent future issues. Additionally, wearing supportive footwear and orthotics can also aid recovery. If you have pain in your heel and calf area, it is suggested that you consult a podiatrist who can accurately diagnose and treat an Achilles tendon injury.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Ahmad Elsamad, DPM of The Institute of Foot & Ankle Reconstructive Surgery . Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our offices located in Merrillville, and Munster, IN . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.