Merrillville, IN
Munster, IN

Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Why Live with Pain and Numbness in Your Feet?
Can Flip Flops Hurt My Feet?
 There are so many different styles of shoes that are available for purchase, but flip flops are often the quick go to and one of the most dangerous to frequently wear. Various foot conditions may develop as a result of wearing flip flops and most can cause severe pain and discomfort. Some of these ailments can include blisters, corns, arch pain, Achilles tendonitis, and most commonly plantar fasciitis or heel pain. It is a natural reaction for the toes to grip the front of the shoe in an effort to have them stay on the feet. This can lead to aching and soreness throughout the entire foot. If flip flops are still your top choice to wear it can be beneficial to rotate them with other styles of flip flops. Sandals that have a strap around the heel can also be less harmful to the feet and it may help to wear high-quality flips flops that are constructed of leather materials. Additionally, it is suggested to refrain from wearing socks with flip flops as this can cause foot strain too. If you have questions about how to choose the right flip flops for you, please consult with a podiatrist.
There are so many different styles of shoes that are available for purchase, but flip flops are often the quick go to and one of the most dangerous to frequently wear. Various foot conditions may develop as a result of wearing flip flops and most can cause severe pain and discomfort. Some of these ailments can include blisters, corns, arch pain, Achilles tendonitis, and most commonly plantar fasciitis or heel pain. It is a natural reaction for the toes to grip the front of the shoe in an effort to have them stay on the feet. This can lead to aching and soreness throughout the entire foot. If flip flops are still your top choice to wear it can be beneficial to rotate them with other styles of flip flops. Sandals that have a strap around the heel can also be less harmful to the feet and it may help to wear high-quality flips flops that are constructed of leather materials. Additionally, it is suggested to refrain from wearing socks with flip flops as this can cause foot strain too. If you have questions about how to choose the right flip flops for you, please consult with a podiatrist.
Flip-flops can cause a lot of problems for your feet. If you have any concerns about your feet or ankles, contact Ahmad Elsamad, DPM from The Institute of Foot & Ankle Reconstructive Surgery . Our doctor will assist you with all of your foot and ankle needs.
Flip-Flops and Feet
Flip-flops have managed to become a summer essential for a lot of people. While the shoes may be stylish and easy to slip on and off, they can be dangerous to those who wear them too often. These shoes might protect you from fungal infections such as athlete’s foot, but they can also give you foot pain and sprained ankles if you trip while wearing them.
When Are They Okay to Wear?
Flip-flops should only be worn for very short periods of time. They can help protect your feet in places that are crawling with fungi, such as gym locker rooms. Athlete’s foot and plantar warts are two common fungi that flip-flops may help protect your feet against.
Why Are They Bad for My Feet?
These shoes do not offer any arch support, so they are not ideal for everyday use. They also do not provide shock absorption or heel cushioning which can be problematic for your feet. Additionally, you may suffer from glass cuts, puncture wounds, and stubbed toes since they offer little protection for your feet.
More Reasons Why They Are Bad for Your Feet
- They Slow You Down
- May Cause Blisters and Calluses
- Expose Your Feet to Bacteria
If you have any questions, please feel free to contact our offices located in Merrillville, and Munster, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Flip Flops and Your Feet
When the weather heats up, you may want to start wearing flip-flops. However, it has been proven that these are not the ideal shoes in terms of preserving the health of your feet.
Flip flops are known to expose your feet to different types of bacteria and fungal infections. When you wear your flip flops in public, you are exposing them to staphylococcus which is a skin-irritating bacterium. Athlete’s foot is also highly contagious and can be spread when you walk around nearly-barefoot.
Another harmful effect of wearing flip-flops is that they develop blisters on the feet. This is because the thin strap rubs against the skin with each step taken. Unfortunately, when blisters pop, they cause you to be more vulnerable to pathogens you pick up by having your feet exposed.
These shoes may also cause “shooting pains”. If you have flat feet, you need arch support to keep your knees, hips, and back in alignment. If you wear flat shoes, your joints are forced to compensate which can cause injuries throughout the body.
If you constantly wear flip-flops, you should avoid doing so as they can lead to many problems for your feet. If you are experiencing any of these foot issues, you should seek help from a podiatrist right away.
Preventing Falls in Children
 Falls are a leading cause of injury for not just older adults, but also for children. In fact, falls are the leading cause of injury in children from birth to about 19 years of age. Falls can result in a variety of foot and ankle injuries, from sprains to fractures and beyond. Fortunately, there are steps you can take to prevent your child from falling and incurring a serious injury. If your child plays on a playground, check the surface under the playground to ensure that it is soft and safe, as well as supervise your child while they play. Make your home safer by using stair gates and guard rails to prevent your child from falling down the stairs. If your child participates in sports, make sure that they wear helmets, padding, or any other safety gear that the sport requires. If your child falls and injures their feet or ankles, take them to see a podiatrist who can diagnose and treat their condition.
Falls are a leading cause of injury for not just older adults, but also for children. In fact, falls are the leading cause of injury in children from birth to about 19 years of age. Falls can result in a variety of foot and ankle injuries, from sprains to fractures and beyond. Fortunately, there are steps you can take to prevent your child from falling and incurring a serious injury. If your child plays on a playground, check the surface under the playground to ensure that it is soft and safe, as well as supervise your child while they play. Make your home safer by using stair gates and guard rails to prevent your child from falling down the stairs. If your child participates in sports, make sure that they wear helmets, padding, or any other safety gear that the sport requires. If your child falls and injures their feet or ankles, take them to see a podiatrist who can diagnose and treat their condition.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with Ahmad Elsamad, DPM from The Institute of Foot & Ankle Reconstructive Surgery . Our doctor will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our offices located in Merrillville, and Munster, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Falls Prevention
Elderly Americans are very susceptible to falls as they get older. Everyone experiences decreases in flexibility, balance, strength, and the senses as they age. This correlates to some eye-opening statistics. 1 in 4 Americans aged 65 and older fall each year. An elderly American is being treated for a fall in an emergency room every 11 seconds. In light of these striking statistics, one can see the importance of taking steps to prevent falls.
Finding an exercise program for the elderly is an excellent way to reduce the likelihood of falls. Look for an exercise program that improves strength and balance. Elderly people who live a more sedentary lifestyle, with little physical activity, are at an increased risk of falling. Wearing well-fitted footwear that provides good foot support and cushion will help prevent falls from poorly fitted shoes. Talking to a podiatrist about your susceptibility to falls and about inspecting your prescriptions will help to avoid any medication that could make falls more likely. Due to a decline in the senses among the elderly, having your eyes and hearing checked is recommended.
Around half of all falls occur in the household. Removing tripping hazards in the home and making it more accommodating to older persons can significantly reduce falls. Some notable household changes include increasing lighting around the house, installing grab bars in the shower and bathroom, and making sure the floor is clear of clutter. Other smart options include installing a shower chair, using rubber-bottomed rugs, and placing railings on both sides of stairwells.
Finally, discuss with a doctor and your family about your fear of falling. This will help to increase awareness among the population on the need for fall prevention. A lack of awareness on the matter, and a downplaying of importance are what increase the risks of falling. Following these tips can help to reduce the risk for yourself and your loved ones.
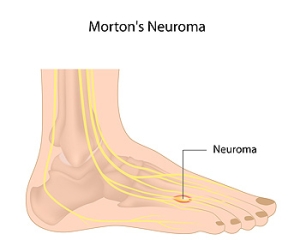
Nerve Growth and Morton’s Neuroma
 Nerve tissue is often affected due to Morton’s neuroma. Growths can form on the tissue, and may cause pressure, pain, and discomfort. Many patients liken the sensation to having a pebble in the shoe, and some people feel a burning or numbing sensation. This condition can develop from repetitive overuse while performing specific sporting activities, or it may come from wearing shoes that do not fit correctly. Additionally, people who have hammertoes, bunions, or flat feet may be prone to developing Morton’s neuroma. Prompt treatment should begin in order to lessen existing pain. It is important to have a proper diagnosis made, which is generally done by having an X-ray, ultrasound, or MRI performed. Relief can be found when shoes that are worn fit properly, in addition to wearing custom made orthotics. There are several treatment options available for Morton’s neuroma, and it is suggested that you consult with a podiatrist who can determine what the best one is for you.
Nerve tissue is often affected due to Morton’s neuroma. Growths can form on the tissue, and may cause pressure, pain, and discomfort. Many patients liken the sensation to having a pebble in the shoe, and some people feel a burning or numbing sensation. This condition can develop from repetitive overuse while performing specific sporting activities, or it may come from wearing shoes that do not fit correctly. Additionally, people who have hammertoes, bunions, or flat feet may be prone to developing Morton’s neuroma. Prompt treatment should begin in order to lessen existing pain. It is important to have a proper diagnosis made, which is generally done by having an X-ray, ultrasound, or MRI performed. Relief can be found when shoes that are worn fit properly, in addition to wearing custom made orthotics. There are several treatment options available for Morton’s neuroma, and it is suggested that you consult with a podiatrist who can determine what the best one is for you.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Ahmad Elsamad, DPM of The Institute of Foot & Ankle Reconstructive Surgery . Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our offices located in Merrillville, and Munster, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton's Neuroma
A neuroma is a thickening of nerve tissue and can develop throughout the body. In the foot, the most common neuroma is a Morton’s neuroma; this typically forms between the third and fourth toes. The thickening of the nerve is typically caused by compression and irritation of the nerve; this thickening can in turn cause enlargement and, in some cases, nerve damage.
Neuromas can be caused by anything that causes compression or irritation of the nerve. A common cause is wearing shoes with tapered toe boxes or high heels that force the toes into the toe boxes. Physical activities that involve repeated pressure to the foot, such as running or basketball, can also create neuromas. Those with foot deformities, such as bunions, hammertoes, or flatfeet, are more likely to develop the condition.
Symptoms of Morton’s neuroma include tingling, burning, numbness, pain, and the feeling that either something is inside the ball of the foot or that something in one’s shoe or sock is bunched up. Symptoms typically begin gradually and can even go away temporarily by removing one’s shoes or massaging the foot. An increase in the intensity of symptoms correlates with the increasing growth of the neuroma.
Treatment for Morton’s neuroma can vary between patients and the severity of the condition. For mild to moderate cases, padding, icing, orthotics, activity modifications, shoe modifications, medications, and injection therapy may be suggested or prescribed. Patients who have not responded successfully to less invasive treatments may require surgery to properly treat their condition. The severity of your condition will determine the procedure performed and the length of recovery afterwards.
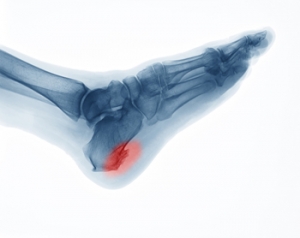
Why Do Heel Spurs Develop?
Heel spurs are the body’s natural reaction to repeated stress placed on the bottom of the heel bone where it attaches to the plantar fascia—the fibrous connective tissue on the bottom of the foot. Heel spurs are actually calcium deposits that build up on the heel bone over time due to tears, strain, and stretching of the plantar fascia, ligaments, muscles, and membrane covering the heel bone. There are several contributing factors to developing heel spurs, and the most common symptoms include pain all around and underneath the heel, inflammation and stiffness that does not get better with rest. If you believe you have heel spurs, make an appointment with a podiatrist for a full examination, diagnosis and proper treatment.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Ahmad Elsamad, DPM from The Institute of Foot & Ankle Reconstructive Surgery . Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our offices located in Merrillville, and Munster, IN . We offer the latest in diagnostic and treatment technology to meet your needs.
Heel Spurs
Heel spurs are the result of calcium deposits that cause bony protrusions on the underside of the heel. Heel spurs are usually painless, but they have the potential to cause heel pain. Heel spurs tend to be associated with plantar fasciitis, which is a condition that causes inflammation of the band of connective tissue that runs along the bottom of the foot. They most often occur to athletes whose sports involve a lot of running and jumping.
Some risk factors for developing heel spurs include running and jogging on hard surfaces, being obese, wearing poorly fitting shoes, or having walking gait abnormalities.
It is possible to have a heel spur without showing signs of any symptoms. However, if inflammation develops at the point of the spur’s formation, you may have pain while walking or running. In terms of diagnosis, sometimes all a doctor needs to know is that the patient is experiencing a sharp pain localized to the heel to diagnose a heel spur. Other times, an x-ray may be needed to confirm the presence of a heel spur.
Heel spurs can be prevented by wearing well-fitting shoes that have shock-absorbent soles. You should also be sure that you are choosing the right shoe for the activity you want to partake in; for example, do not wear walking shoes when you want to go on a run. Additionally, maintaining a healthy weight can be beneficial toward preventing heel spurs, as it will prevent an excess amount of pressure being placed on the ligaments.
There are a variety of treatment options for people with heel spurs. Some of these include stretching exercises, physical therapy, shoe inserts, or taping and strapping to rest stressed muscles and tendons. If you have heel pain that lasts longer than a month, don’t hesitate to seek help from a podiatrist. Your doctor can help you determine which treatment option is best for you.